Antonina Wojcik, MS, CGC (she/her); Katie Lang, MS, CGC (she/her); Deepti Babu, MS, CGC (she/her)
It’s Deepti here – I have a confession to make. It wasn’t until I first joined the NSGC Board that I fully appreciated how NSGC’s Federal bill advocacy efforts intersect with justice, equity, diversity, and inclusion (J.E.D.I.) efforts. Up to that point, particularly from my vantage point as a genetic counselor practicing outside the U.S., I thought these issues were mutually exclusive. But I was mistaken. Since others might similarly misunderstand, I thought it’d be helpful to shine light on this connection. To ensure we stay firmly in the facts, I’ve called in two experts for help – Antonina Wojcik and Katie Lang, Chair and Vice-Chair (respectively) of NSGC’s Advocacy Coordinating Committee (ACC). Antonina, Katie, and I are collaborating on this piece to help us understand exactly how connected Federal advocacy and J.E.D.I., two pillars of NSGC’s 2022-2024 Strategic Plan, are.
At their root, the “why” is the same.
Let’s start by getting into the “why” for each initiative, at a high level.
This is a complex issue that can’t be addressed in full here, but at its root, NSGC’s Federal bill, the Access to Genetic Counselor Services Act, aims to grant Medicare beneficiaries coverage for genetic counselor services. The federal agency that manages Medicare, the U.S. Centers for Medicare and Medicaid Services (CMS), does not recognize certified genetic counselors as health care providers and, thus, does not reimburse for our services. (Of note, CMS recognizes other providers who provide genetic counseling). As a result, many individuals in the U.S. who need genetic counselor services cannot get them unless they have other means (like supplemental insurance coverage or the ability to pay out of pocket). This gap in reimbursement has other negative impacts, including to the genetic counseling workforce and job market, but we’re hoping to cover that in a future Advocate article.
This is another complex issue that can’t be fully addressed here, but at its root, NSGC’s J.E.D.I. efforts advocate for underserved and historically excluded populations, within and outside our organization. That includes those we strive to serve, to bring health equity and access (including reimbursement) to genetic counselor services to all who need it. The reality is that not every person who stands to benefit from speaking to a genetic counselor gets to do that. Barriers to access include being under/uninsured, lack of geographic access to a genetic counselor, or a lack of awareness about genetic counselors because of health care disparities embedded throughout the broader system. As a result, many individuals in the U.S. who need genetic counselor services cannot get them unless they have other means. This gap has other negative impacts, including how underrepresented individuals learn about and consider joining our field if payment for genetic counseling services and job opportunities are challenged.

In their simplest forms, both initiatives have the same “why”: to close gaps that underserved individuals face with getting the genetic health care services that they need.
Data points help to tell the story
Medicare is the largest health care payer in the U.S. – it covered 62 million people in 2020, which represented 19% of the population, and is growing.1,2 In the U.S. individuals with private health insurance typically receive it through their employer as a benefit or they pay out of pocket for an insurance plan. Those who lose their job or cannot afford a plan may qualify for other programs like Medicaid, but many end up without health insurance or under-insured.
Medicare is different. Why? Because most people qualify for Medicare by turning 65, meaning Medicare is a system you age into, rather than afford based on income. This makes Medicare a far more equitable system of health insurance. The numbers speak for themselves. In the U.S., the 2021 uninsured rate for individuals aged 18-64 was 10.2%. The uninsured rate for those over age 65? Less than 1%!3 For millions, enrolling in Medicare means having stable health insurance, or any health insurance, for the first time. In fact, studies show improved health trends in uninsured individuals after enrollment in Medicare.4 Given these staggering numbers, it is fair to think of Medicare as a system that opens doors to health care that were previously closed for many in the U.S.
So how does this relate to genetic counselors? If our goal is to provide care to all patients who need our services, especially those who face barriers and are underserved5, data can help tell the story. Let’s compare three lists: states with the most genetic counselors per the NSGC 2022 Professional Status Survey, states with the highest percentage of Medicare beneficiaries who are living below the Federal poverty line, and states with the most Medicare beneficiaries who report any of the following as their race and/or ethnicity (often underrepresented identities): Alaska Native, American Indian, Asian, Black, Hispanic, Multiple Races, Native Hawaiian, or Pacific Islander (persons of Hispanic origin may be of any race; all other racial/ethnic groupings are non-Hispanic). Quick note: we acknowledge that there are many other underrepresented dimensions in populations that also intersect; we are limiting our discussion to race and ethnicity.
When we do that, as shown in the diagram, we find that states with underserved Medicare beneficiaries are not the same states where most genetic counselors are.6-8
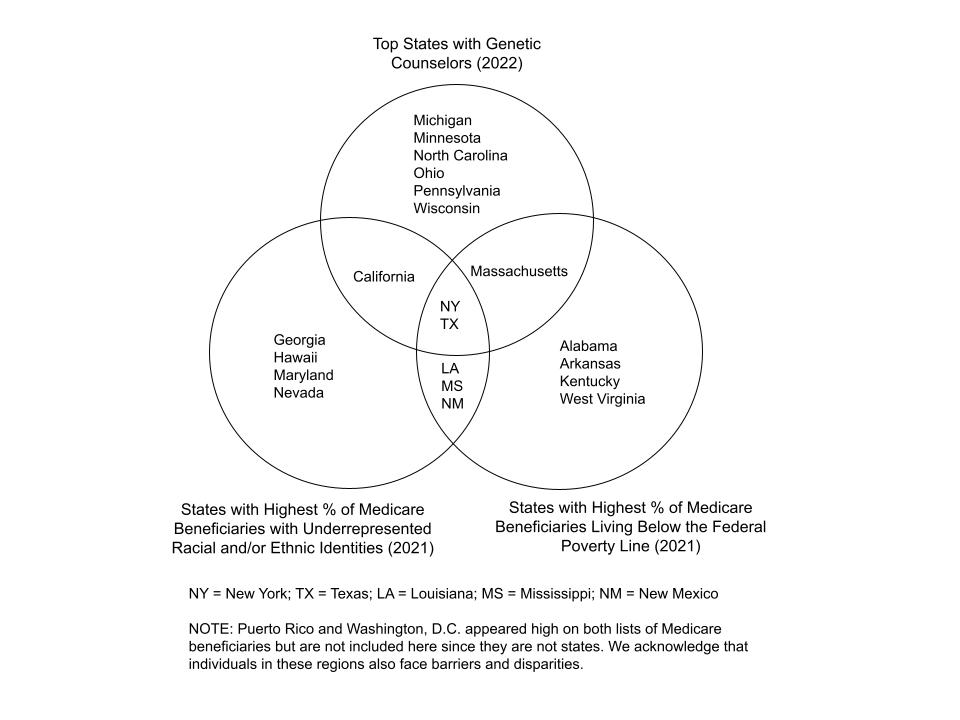
Only two states, New York and Texas, have a high concentration of genetic counselors and high percentages of underserved Medicare beneficiaries. This is a huge opportunity for us as a profession to meet the health care needs of millions of individuals.
So how does our Federal bill help? By increasing access to genetic counselor services for patients with Medicare, we can reach those we have historically underserved and excluded. If our services are not covered for these patients, it may not be possible for genetic counselors to operate sustainable genetic counseling practices in these areas, within institutions or privately. Until the Access to Genetic Counselor Services Act passes, patients who reach the age of Medicare eligibility still don’t have coverage for genetic counselor services, even though they may finally be able to access other aspects of health care. Of course, it’s unacceptable for any patient to have to wait until they turn 65 to gain access to genetic counselors, but our bill is one huge step towards health equity. While one bill does not resolve all the inequities, disparities, and problems within genetics and genetic counseling, it would still be immediately impactful for millions of patients.
A “two-for-one” when you support Federal advocacy efforts
Hopefully, by seeing the common “why” and facts that underpin these issues, it’s clearer how tightly linked NSGC’s Federal Advocacy and J.E.D.I. efforts are. As a profession, we can put our support behind these initiatives that further access to genetic counselor services for those who need it, particularly those who already face disparities across the health care system. By giving your time and energy to NSGC’s Federal advocacy efforts, you are also helping to advance J.E.D.I. for the communities we strive to serve.
Wondering how to help? Here are 3 things:
- Register for a virtual meeting with your Member of Congress using the link here or scan this QR code.
- A member of the NSGC team will join the meeting to support you. If you need resources to prepare, they are found at the link here.
- Tap into your professional and personal networks to gain support for the bill.
- An organization can sign on to support by using the link here.
- Watch Antonina’s video using the link here for more details on plans for 2023.
Have an idea or questions? Email advocacy@nsgc.org and a member of the Advocacy Coordinating Committee will be happy to connect with you.
References
- Kaiser Family Foundation. “Medicare Beneficiaries as a Percent of Total Population.” Timeframe: 2020. Available from https://www.kff.org/medicare/state-indicator/medicare-beneficiaries-as-of-total-pop/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed February 27, 2023.
- MedPAC. Report to the Congress: Medicare and the Health Care Delivery System. “Chapter 2: The next generation of Medicare beneficiaries.” June 2015. Available from https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/chapter-2-the-next-generation-of-medicare-beneficiaries-june-2015-report-.pdf Accessed February 23, 2023.
- Tolbert J, Drake P, Damico A. Kaiser Family Foundation. “Key Facts about the Uninsured Population.” Available from https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/. Accessed February 23, 2023.
- McWilliams JM, Meara E, Zaslavsky AM, et al. Health of previously uninsured adults after acquiring Medicare coverage. JAMA. 2007;298(24):2886-94. doi: 10.1001/jama.298.24.2886. PMID: 18159058.
- Suther S and Kiros G-E. Barriers to the use of genetic testing: A study of racial and ethnic disparities. Genet Med. 2009;11:655-662. doi: https://doi.org/10.1097/GIM.0b013e3181ab22aa. PMID: 19752639.
- Kaiser Family Foundation. “Distribution of Medicare Beneficiaries by Federal Poverty Level” Timeframe: 2021. Available from https://www.kff.org/medicare/state-indicator/medicare-beneficiaries-by-fpl/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Under%20100%25%22,%22sort%22:%22desc%22%7D. Accessed February 23, 2023.
- Kaiser Family Foundation. “Distribution of Medicare Beneficiaries by Race/Ethnicity.” Timeframe: 2021. Available from https://www.kff.org/medicare/state-indicator/medicare-beneficiaries-by-raceethnicity/?currentTimeframe=0&selectedDistributions=white&sortModel=%7B%22colId%22:%22White%22,%22sort%22:%22asc%22%7D. Accessed February 23, 2023.
- National Society of Genetic Counselors. “2022 Professional Status Survey.” Available from https://www.nsgc.org/Policy-Research-and-Publications/Professional-Status-Survey. Accessed February 23, 2023
Antonina Wojcik, MS, CGC (she/her) is the 2023 NSGC Advocacy Coordinating Committee Chair. Antonina is a laboratory genetic counselor specializing in somatic oncology. She is dedicated to supporting the growth and sustainability of the genetic counseling profession by engaging in advocacy and public policy work.
Katie Lang, MS, CGC (she/her) is the 2023 NSGC Advocacy Coordinating Committee Vice Chair. Katie is the Director of Cancer Genetic Counseling at Vanderbilt University. She is passionate about helping fellow genetic counselors engage with the legislative process at both the state and federal levels.
Deepti Babu, MS, CGC (she/her) is 2023 NSGC President and Founder of Integrity Content Consulting. Deepti's engagement with NSGC spans 25 years, since joining as a student member and catching the volunteerism bug. She enjoys making meaning of complex scientific topics for varied audiences through her medical writing.